We have BIG NEWS.
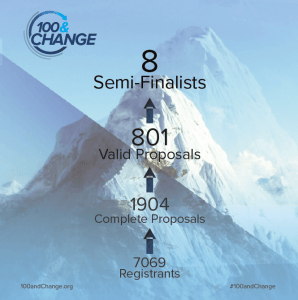
This past summer, we applied for the MacArthur Foundation’s 100 & Change competition, a contest in which one applicant will be awarded 100 million dollars to solve “a critical problem of our time”. In case you didn’t catch that number, we’ll repeat: one hundred million dollars towards the philanthropic or academic venture of your choosing.
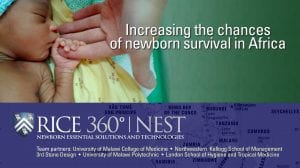
As mentioned, Rice 360° and our incredible partners (below) applied to this contest many months ago. We were very excited to have been invited to continue to the next round of applicants in December.
After biting our nails in anticipation for a month, we just received the exciting news that we are now one of 8 semi-finalists for this crazy prestigious award!! One million thanks to the MacArthur Foundation for keeping us in consideration!
But, in the middle of our ecstatic celebration, it dawned on us the frightening responsibility that comes with this news. We have the chance to bring our mission to scale — ensuring a baby born in Africa has the same chance of survival as one born in the United States. Current rates of progress show it will take more than 150 years to end preventable newborn deaths in Africa. We have the chance to cut that down to 10 years with our proposal: NEST.
What’s the challenge? In Africa, 85% of small and sick babies die from infection, being born too soon, or complications during labor and delivery. The vast majority of these deaths can be prevented using solutions currently not available in the country.
What’s NEST? NEST stands for Newborn Essential Solutions and Technologies. It’s a set of 17 technologies already used in NICUs in the United States that help babies breathe, keep them warm, and manage infections. What makes this suite of technologies unique is that it’s both affordable and rugged enough to withstand the harsh environment of low-resource areas. Too often, medical devices are given to hospitals in Africa that aren’t made to deal with power surges, humidity, and inconsistent water access. We keep these issues in mind when designing NEST.
How are students involved? We work with clinicians in Malawi to determine what medical devices they need to do their jobs most effectively. Rice students receive those problems as design challenges. They come up with a design solution and get feedback from these clinicians in the field during summer internships. Our students, like many college kids, want to save the world. We try to give them the experience and skills to develop solutions to do that.
What does success of this project look like? Like the title of this post suggests, we hope to save a million small and sick babies and inspire a million hearts and minds. In addition to ending preventable newborn death in Malawi and the rest of sub-Saharan Africa, we intend to establish an education program to develop the next generation of inventors and entrepreneurs, starting with the students Matt works with at The Poly. Local ownership of frugal innovation is the ultimate goal. We like to think of it as an innovation ecosystem.
“Continent-wide change may sound impossible, but our team is made up of realists, who have more than 150 years combined experience in global health. Each and every one of us knows this is within reach. We can see the finish line, and we are committed to getting there.”
-Rebecca Richards-Kortum
We are so grateful for our incredible team below. Check out their awesomeness!
Joy Lawn has lived and worked in many African countries, including as a lecturer and neonatalogist in Ghana in the 1990s. She shifted to public health and global estimation working at the WHO Collaborating Center at the CDC , and then at the Institute of Child Health in London, completing a Masters of Public Health at Emory University and a PhD in perinatal epidemiology at University College London. For ten years she was been Director Global Evidence and Policy for Gates Foundation funded Saving Newborn Lives (SNL) programme of Save the Children, working with governments and partners to scale up and evaluate newborn care including leadership in the Every Newborn Lancet series and Action Plan.
Queen Dube, MBBS, MMed, is a Consultant Pediatrician and Clinical Head of the Department of Pediatrics at Queen Elizabeth Central Hospital in Blantyre, Malawi. She trained for her medical degree in Britain and is one of only eight pediatricians in Malawi’s government health system. Her research has focused on pediatric HIV, neonatal sepsis, neonatal meningitis, malaria, and nutrition.
Kara Palamountain is a Research Associate Professor at the Kellogg School of Management (KSM). Her primary area of interest is the development and adoption of medical technologies in Africa. She has managed over 50 KSM research teams conducting market entry analysis in over a dozen countries. She is also the President of the Northwestern Global Health Foundation.
Theresa Mkandawire, is currently the Dean of Faculty of Engineering and an associate professor of civil engineering at the University of Malawi Polytechnic. She holds a PhD in water engineering obtained from Leeds Metropolitan University, UK and a Master of Science degree in Environmental Engineering obtained from Oklahoma State University. Theresa’s areas of specialization are water quality, water supply and sanitation, wastewater treatment and Water Resources Management.
Hannah Blencowe is a Faculty of Epidemiology and Population Health in the Department of Infectious Disease Epidemiology at the London School of Hygiene and Tropical Medicine (LSHTM). Her background is in medicine, having worked as a clinician in pediatrics, general practice and obstetrics, and gynecology. Her research work is focused around improving the measurement and global estimation of perinatal conditions (including preterm birth, low birthweight, stillbirths, congenital abnormalities and neonatal morbidity) as part of the Every Newborn Action plan to end preventable newborn deaths and stillbirths.
Liz Molyneux is a British pediatrician at the College of Medicine, and Queen Elizabeth Hospital/College of Medicine in Blantyre, Malawi. She and her husband went to Malawi in 1974 and they have spent over 30 years living and working there. They first worked at a district mission hospital before being requested to move to the central government hospital. Elizabeth’s interests are wide and varied; having spent 10 years in Alder Hey Liverpool UK in oncology and then as clinical director of the emergency unit, she has maintained these interests in Malawi. With WHO she has developed the Emergency Triage Assessment and Treatment course based on the Advanced Pediatric course of the UK of which she is a founder member. Infectious diseases and tropical oncology are areas of clinical research but health care delivery in a resource-constrained setting is a major interest.
Josephine Langton, Academic Head of Department for the Paediatric and Child Health Department at the College of Medicine, trained at Birmingham University, England. A former doctor at National Health Service, Josephine is currently a Paediatric Emergency Medicine Consultant at Queen Elizabeth Central Hospital in Blantyre, Malawi. With special interests in medical education, qualitative research and quality improvement, Josephine believes children across the world are our future and it is our responsibility to provide them with good healthcare services.
Robert Miros is the CEO of 3rd Stone Design Inc., a privately held product design and development company engaged in engineering, manufacturing, and product strategy. Miros is a prolific inventor with over 30 granted patents to his name. 3rd Stone Design has collaborated with Rice 360° for the past 7 years on five different global health technologies.
As an undergraduate bioengineering student at Rice University, Jocelyn Brown invented the Pumani bCPAP, a low-cost respiratory device designed to help newborns in low-resource hospitals survive respiratory distress. After graduating, she relocated to Malawi to evaluate the Pumani bCPAP and scale it to all government hospitals in the country. As the current Product Manager for Medical Devices at 3rd Stone Design, she interfaces daily with engineers, manufacturers, and customers to provide a Pumani bCPAP that meets the needs of newborns around the world.
Malawian-born Gregory Gamula studied Electrical Engineering at the University of Malawi Polytechnic. Prior to receiving a Doctor of Engineering (Energy and Environment) at China University of Geosciences, he attained a Master of Science in Renewable Energy from the University of Oldenburg, Germany. A registered engineer with the Malawi Board of Engineers, Gregory currently serves as Deputy Dean of Engineering, University of Malawi Polytechnic.
Want to know even more? Check out the other 100&Change candidates. Click here.
Stay tuned for more updates on our NEST progress and thanks for reading!
Emily Mooney